Osteoporosis is a silent disease, it affects millions of people worldwide, causing weakening of the bones making it brittle and fragile. While it is a major health concern, especially for older adults there is a lack of awareness and understanding. Bone health is ignored until someone ends up with a fragility fracture (hip, spine, and wrist fractures due to simple falls).
What is Osteoporosis?
Osteoporosis occurs when the body loses too much bone tissue or does not produce enough new bone. This weakens your bones- in other words makes the bone more porous! This makes the bone prone to fractures.
What we do not realise is that bone is not a constant structure. Like any other organ or tissue bone is continuously undergoing changes in response to many factors. At an early age, the bone formation is faster and higher causing build-up of bone. This happens till the age of 30-35. This is called the age of ‘peak bone mass.’ Consider this as a deposit in the bank. As we age the bone loss is higher than formation. So, a person with higher peak bone mass is less likely to get osteoporosis than a person who has lower peak bone mass.
What are the risk factors for osteoporosis?
There are multiple risk factors- some are modifiable, and some are not modifiable factors.
Age, sex, and family history- the older a person is the higher the risk for osteoporosis, women are more likely to get osteoporosis than men, parent or a sibling with osteoporosis or a fragility fracture puts you at a higher risk.
Modifiable factors- low Calcium and Vit D intake, sedentary lifestyle, smoking, and alcohol consumptions.
Some medical conditions and certain drug use can also put a person at a risk of developing osteoporosis.
What are the symptoms of osteoporosis?
1. Back pain
2. Loss of height
3. Stooped posture
4. Fractures (wrist, spine, hip)

Diagnosis of Osteoporosis:
A bone density test is done to assess strength of the bone- in other words to assess if the bone has become more fragile and prone to fractures
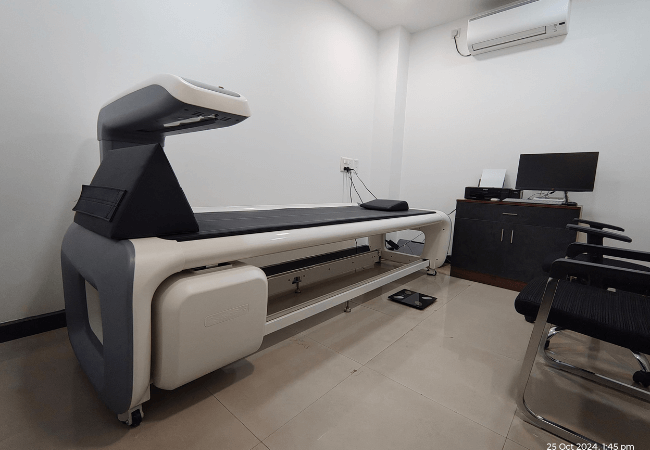
This test takes a few minutes and uses a minimal dose of x-rays to assess the mineral content of the bone. It is safe and the dose of a scan is generally less than that of a regular x-ray.
The bones that are normally tested are in the lumbar spine, hips and sometimes the forearm.
This is called a DEXA scan- Dual energy x-ray absorptiometry scan.
What is the use of a DEXA scan?
A DEXA scan can also be used to assess the fat distribution in the body. It can be used to estimate the fat in the subcutaneous layers that is below the skin and visceral adipose- that is around the organs. This can be a useful assessment for people who are planning diet and exercise regimens for weight loss.
A DEXA scan is also known by other names- bone mineral density test, BMD test, DXA; Dual-energy x-ray absorptiometry scan, Bone densitometry, Dual x-ray absorptiometry.
Who needs to get a DEXA scan?
Women over the age of 60 need to get a bone density scan. Women who are menopausal are at high risk of losing bone mass which can lead to fractures. Men above the age of 65 may develop osteoporosis as well and are suggested a baseline assessment with a DEXA.
Women or men of other ages with other risk factors may also be suggested a DEXA scan for evaluation of bone density if-
Complications:
Hip fractures and spine fractures are the most serious complications of osteoporosis. These fractures, often caused by simple falls at home can cause considerable disability. Hip fractures are also known to increase the risk of death within the first year of injury.
In some patients’ spine fractures may occur without having a fall. The bones may weaken to the point of collapsing. This can cause back pain, hunched posture, and loss of height.
Meet an orthopedic surgeon to understand your risk of osteoporosis and get evaluated.